Dynamic Health IT (DHIT) was in attendance for the Da Vinci FHIR Connectathon hosted by GuideWell (parent company of Florida Blue) in Jacksonville Florida. For those of you not familiar, the Da Vinci Project is a collaboration of trail-blazers in the healthcare space who are looking to revolutionize information sharing. It is a private sector initiative comprised of experts from some of the largest and most prestigious payer, provider and vendors in the healthcare marketplace. Their goal is to accelerate the adoption of HL7® FHIR® as the standard to support and integrate data exchange for value-based care (VBC) with a focus on provider/payer data exchange.
The Connectathon featured three different tracks. We participated in the Clinical Reasoning Track, which focuses on exploring the use of FHIR to calculate Clinical Quality Measures (CQMs). As we’ve contributed to this track, we’ve also increased our understanding of issues related to migrating to FHIR-based CQMs. For DHIT, this means the integration of separate products – Dynamic FHIR Server with CQMsolution.
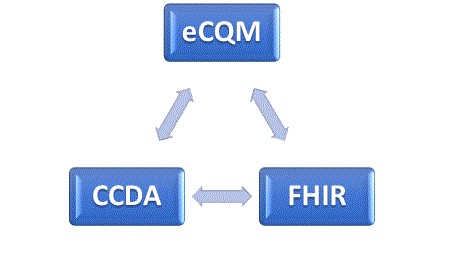
As it stands today, FHIR data types are not used in the calculation of eCQMs. (eCQMs are the Clinical Quality Measures generated directly from EHR data with no intervening manual abstracting process). But Da Vinci members are looking to obsolete the Quality Data Model (QDM) data elements currently used for calculation and presentation in the QRDA Cat I files and replace them with FHIR. A FHIR Measure Report could replace the QRDA Cat I and QRDA Cat III files. FHIR also offers new operations that instruct the FHIR server to perform measure calculation. Tangentially, DHIT has explored the use of the 2.1 CCDA as a data source for calculating eCQMs (more on that later).
The Clinical Reasoning Track is evolving as well. Previous iterations used “normal” QDM-based eCQMs but relied on FHIR patient data that was converted using QDM to QI Core Mappings. Developers have been hard at work doing a trial run to populate existing eCQMs by using FHIR data types. This will make it possible to run FHIR-based eCQMs against FHIR data elements.
DaVinci has expanded this track include additional operations related to submitting and collecting data. These include the submission of data from the producer to the consumer. In this scenario, an EHR might submit data directly to a Payer. Additionally, consumers can request data from the producer using a “Collect Data” operation or subscribe to the producer’s Subscription Service to be notified when CQM data becomes available. All of these operations limit the scope of data collected to what is required by the measures.
During this Connectathon we focused on one CQM – Venous Thromboembolism Prophylaxis (VTE-1). Some of the issues we faced were the sheer scope of changes required to begin this process. For example, the version of the CQL language itself differs between the current CMS version of the measure and the newly released FHIR version of the measure. In the end Dynamic Health IT was able to make considerable progress towards the goal of the track.
Back to the challenge of using the 2.1 CCDA as a data source for calculating eCQMs: Based on our research to-date, many current eCQMs cannot be accurately calculated from standard 2.1 CCDA data elements. NCQA offers an eCQM certification process that involves calculating quality measures from CCDA documents but it only includes a subset of the MIPS/QPP eCQMs and some are older definitions. Why is this? We suspect it is because the remainder are problematic to calculate from a CCDA.
There are several reasons for this:
- Many measures include exceptions and exclusions and these are not captured in a standard CCDA. For example, skipping a Breast Cancer screening for a woman with bi-lateral mastectomies would be an exclusion. “Patient refused to get a flu shot” would be an exception. Calculating eCQMs without exceptions and exclusions is possible but will result in an inaccurate and lower score.
- A typical 2015 Edition Certified 2.1 CCDA (the kind produced by most EHRs) lacks a standard representation for the Adverse Event used by CMS347v2 (Statin Therapy).
- Some measures call for Assessments but there’s no standard way to convey the result of the Assessment in the CCDA.
DHIT’s flagship product ConnectEHR is certified for CCDA creation. We are currently working with HL7 to expand the CCDA data elements to accommodate more of the eCQM measure requirements. Most current adjustment to CCDA is related to negation. There are also other issues relate to using a CCDA as a data source, such as values being provided as free-text, rather than being codified and different EHR systems capturing the same clinical values/events in different ways. Despite these obstacles, we continue to pursue the eCQM data capture challenge and look forward to participating in the next Connectathon in Atlanta. Hope to see you there!



