The Centers for Medicare & Medicaid Services (CMS) released the CY 2026 Medicare Physician Fee Schedule (PFS) final rule on October 31, 2025. While the rule covers broad payment updates, its most significant impact lies in the Quality Payment Program (QPP)—particularly the evolution of the Merit-based Incentive Payment System (MIPS) and its quality reporting requirements.
The 2026 Medicare Physician Fee Schedule (PFS) final rule maintains the 75-point performance threshold for MIPS. It also calls for:
- A new mandatory payment model for heart failure and low back pain – Ambulatory Specialty Model (ASM)
- Telehealth: Several pandemic-era telehealth flexibilities have been made permanent
- Expansion/refinement of MIPS Value Pathways (MVPs)
Here’s the URL if you want to dive into the details.
This blog will focus specifically on MIPS and CQM reporting changes.
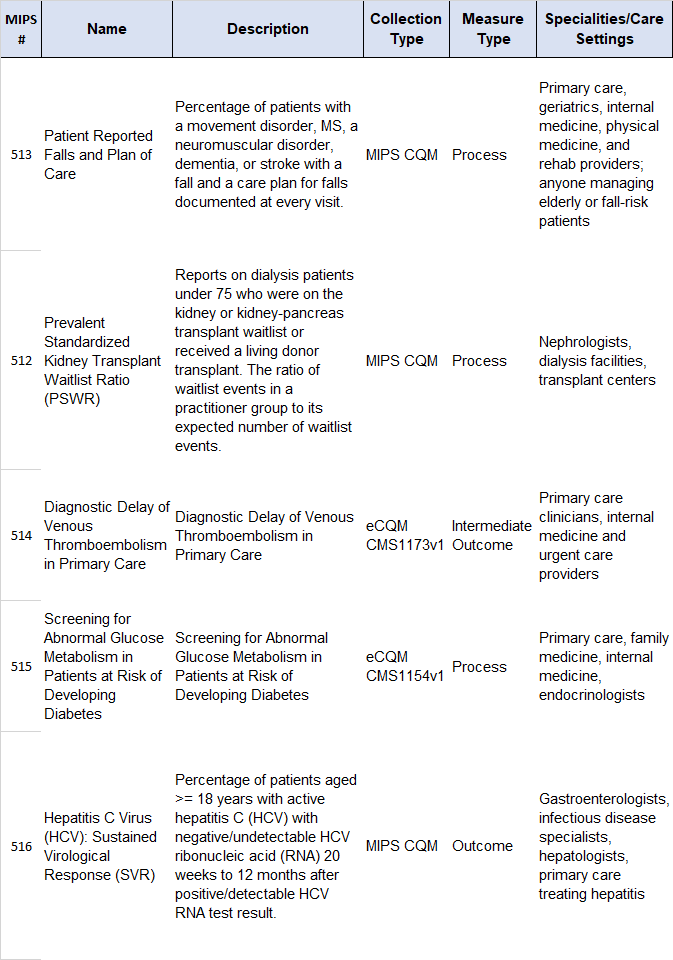
New Quality Measures:
Removed Quality Measures:
No eCQMs have been removed. Just MIPS CQMS:
- 185 Colonoscopy Interval for Patients with a History of Adenomatous Polyps – Avoidance of Inappropriate Use
- 264 Sentinel Lymph Node Biopsy for Invasive Breast Cancer
- 290 Assessment of Mood Disorders and Psychosis for Patients with Parkinson’s Disease
- 322 Cardiac Stress Imaging Not Meeting Appropriate Use Criteria: Preoperative Evaluation in Low-Risk Surgery Patients
- 419 Overuse of Imaging for the Evaluation of Primary Headache
- 424 Perioperative Temperature Management
- 443 Non-Recommended Cervical Cancer Screening in Adolescent Females
- 487 Screening for Social Drivers of Health
- 498 Connection to Community Service Provider
- 508 Adult COVID-19 Vaccination Status
MVP Rollout
CMS updated all 21 existing MVPs and introduced 6 new MVPs for 2026:
- Diagnostic Radiology
- Interventional Radiology
- Neuropsychology
- Pathology
- Podiatry
- Vascular Surgery
Additionally:
- Practices will self-attest to their specialty composition (single specialty or multispeciality group that meets small practice requirements) during MVP registration.
- Multispeciality small practices can report an MVP as a group
- Subgroup reporting remains optional in 2026
- Beginning with the 2026 performance period, QCDRs and qualified registries (QRs) must support MVPs applicable to the MVP participant on whose behalf they submit MIPS data within 1 year of MVP finalization. In addition, they must support all measures and activities that are included in the MVP. This will be a challenge for participants whose EHR vendors lack support for key data elements required by MIPS measures. EHR vendors that self-nominate as a QCDR or qualified registry are required to support all measures within each applicable MVP.
Promoting Interoperability (PI)
- The Electronic Case Reporting (eCR) measure is currently required for 2026. (It was suppressed for 2025 due to the CDC’s hiatus in onboarding new participants.) CMS reports that they will continue to work with the CDC to assess whether the eCR measure warrants suppression for 2026. Important: For 2025, you must still attest as to Option 1, Option 2, or an applicable exclusion. The measure will no longer be scored, but it is still required.
- Security Risk Analysis measure will require an additional attestation confirming that clinicians conducted risk management activities, as outlined under the HIPAA Security Rule.
- SAFER Guide: Clinicians must use the updated 2025 Safety Assurance Factors for EHR Resilience (SAFER) Guide in place of the 2016 version for their self-assessments under the High Priority Practices measure.
- A new bonus measure has been added to promote interoperability, providing for public health data exchange using the Trusted Exchange Framework and Common Agreement (TEFCA). It’s one of four available bonus measures under this objective, in which a maximum of 5 points can be earned if reporting one, more than one, or all optional bonus measures.
ACOs
Accountable Care Organizations (ACOs) participating in the Medicare Shared Savings Program (SSP) are required to report quality data using the Alternative Payment Model (APM) Performance Pathway (APP) Plus quality measure set. The standard APP quality measure set is no longer available to SSP ACOs for reporting.
Key details regarding quality reporting options for ACOs in CY 2026:
- Mandatory Measure Set: SSP ACOs must use the APP Plus quality measure set.
- Data Submission Methods: ACOs have the option to report quality data via electronic Clinical Quality Measures (eCQMs) or MIPS Clinical Quality Measures (MIPS CQMs).
- Incentives for eCQMs: CMS continues to offer the eCQM/MIPS CQM reporting incentive, which provides an upward adjustment to an ACO’s quality performance category score when they report quality data using eCQMs, helping them meet the quality performance standard and share in maximum savings.
- Removed Measure: The rule finalizes the removal of the “Screening for Social Drivers of Health” measure (Quality ID: 487) from the APP Plus quality measure set.
For ACOs reporting Medicare CQMs, CMS has revised the definition of eligible beneficiaries beginning in performance year 2025 and for subsequent years. Under this policy, a beneficiary would be considered eligible if they received at least one primary care service during the applicable performance year from an ACO clinician. This change is intended to increase alignment with the ACO’s assignable population, simplifying patient matching and reducing administrative burden.
How Dynamic Health IT Can Help
If you’ve made it to the end of this blog, you know that MIPS (and especially PI and CQM reporting) is always a moving target. Partner with DHIT to transform your CQM reporting from a complex burden into a painless process.