Each year, there are a host of changes to clinical quality measure logic, reporting requirements and CMS quality program policy. Come 2019, the usual cycle of CQM turnover is joined by an overhaul of CQM logic methodology: Clinical Quality Language (CQL).
In our previous post, we discussed 2018 changes. In this post, we’ll handle the changes coming for the 2019 Reporting Year. Those fall into five categories:
- CQL transition: Clinical Quality Language (CQL) is a measure authoring language standard that will replace the measure logic previously defined by the Quality Data Model (QDM) and QDM in 2019.
- Value Set Changes: changes to official codes and code sets used by CMS quality measures
- Measure Specification and Logic Changes: changes in the manner of calculation and/or specific codes and code sets included in each measure
- QRDA-I/III reporting format changes: changes in the XML requirements (QRDA-I or QRDA-III) for major CQM reporting programs (such as MIPS, HQR and Joint Commission)
- Reporting changes: High-level program changes such as menu and number of required of measures, method of reporting, etc.
CQL transition
The conversion of eCQMs to Clinical Quality Language (CQL) has been a hot topic ever since CMS announced that, starting with the 2019 reporting period, eCQMs would move from logic based on an HQMF XML modeling language to CQL. In little more than two months, CQL will become the lingua franca of eCQMs.
CQL has been chosen for its ability to give quality measure authors more flexibility in creating precise definitions of quality measures that are human readable. But what does this mean for health care providers and EHR vendors? If implemented smoothly, it should be barely noticeable by providers. Measure changes between 2018 and 2019 will be absorbed by the CQL measures and calculated as expected, versions notwithstanding.
The impact on EHR developers is far more significant. While developers providing calculation and analysis tools based on CQL have flexibility to use the files that integrate best into their software (ie, ELM vs JSON), they will need to overhaul their measure specifications at the root level to ensure they are using a CQL basis.
CQL makes calculation logic more readable and transparent. For example ability to calculate within the logic itself. Previously, a concept like “cumulative medication duration” was a derived
element that could not be expressed with QDM-based logic. CQL expresses this kind of calculation in a computable format within the logic.
Fortunately, DHIT has rendered eCQMS (and a wide range of non-eCQMs) in JSON well in advance of the 2019 reporting deadlines.
Value Set Changes
As discussed in Part 1, there are annual value set changes that affect eCQMs differently each reporting year. The National Library of Medicine (NLM) maintains the Value Set Authority Center (VSAC), which releases value set updates annually. The entirety of these value set changes are incorporated into our CQMsolution application each release year, with backward compatibility maintained for previous reporting years. The only way to fully implement these changes is to be sure that value sets and their respective codes crosswalk perfectly to the VSAC release.
Measure Specification and Logic Changes
Each new reporting year brings a new batch of measure versions. The United States Health Information Knowledge base (USHIK) offers a comparison tool for visualizing changes in measures across years. The tool is accessible directly from the eCQI Resource Center, but as of this writing is not yet accessible for 2019 eCQMs. Changes to the measure specifications can range from adjusted wording in the measure overview to an adjustment to how a measure population is calculated and its data elements. Examples of new data criteria include the attributes ‘prevalencePeriod’ and ‘components.’
QRDA-I/III reporting format changes
Here is a rundown of the most relevant changes to the requirements in QRDA-I and QRDA-III submission files:
QRDA-I:
- Changes to accepted date time formats: made more expansive
- Data types of CD or CE SHALL have either code or nullFlavor but not both
QRDA III:
- Changes to group-level reporting identification (for MIPS-Group and MIPS Virtual Groups). MIPS Groups will use such that it SHALL be the group’s TIN, while the virtual group will use its Virtual Group Identifier
- Changes across the XML to support transition from ‘ACI’ to ‘Promoting Interoperability’
- Standard measure identifier changes (UUIDs)
Reporting changes
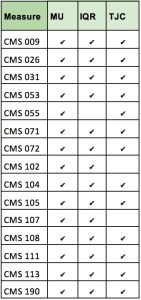
The overall list of CMS eCQM measures in 2019 will stay the same for hospitals, but there are a few program-level measure adjustments for hospitals:
On the EP/EC side, there are some changes to the overall menu of measures:
- CMS 249 and CMS 349 are added
- CMS 65, CMS 123, CMS 158, CMS 164, CMS 167, CMS 169 are removed
- CMS166 -previously for Medicaid-only submission – has been phased out.
Reporting for eligible clinicians has expanded to include the use of the MIPS-API, which has undergone evolution since introduction in 2018.
One significant change on the hospital side is that a QRDA-I submitted and accepted into production will overwrite any preexisting file based on the exact match of five key elements identifying the file: CCN, CMS Program Name, EHR Patient ID, EHR Submitter ID, and the reporting period specified in the Reporting Parameters Section.
For those submitting Joint Commission eCQMs, the program will be shifting to the Direct Data Submission (DDS) Platform, in which hospitals will submit measures directly. DHIT will offer a full suite of consulting and data review services to support this.