The Quality Payment Program (QPP) continues to evolve towards enhanced healthcare quality and efficiency. The 2025 Final Rule introduces several noteworthy changes and updates that will impact both Merit-based Incentive Payment System (MIPS/traditional MIPS) participants and Alternative Payment Models (APMs). Here’s a comprehensive overview of the upcoming changes and what they mean for healthcare providers.
Key Changes in the 2025 QPP Final Rule
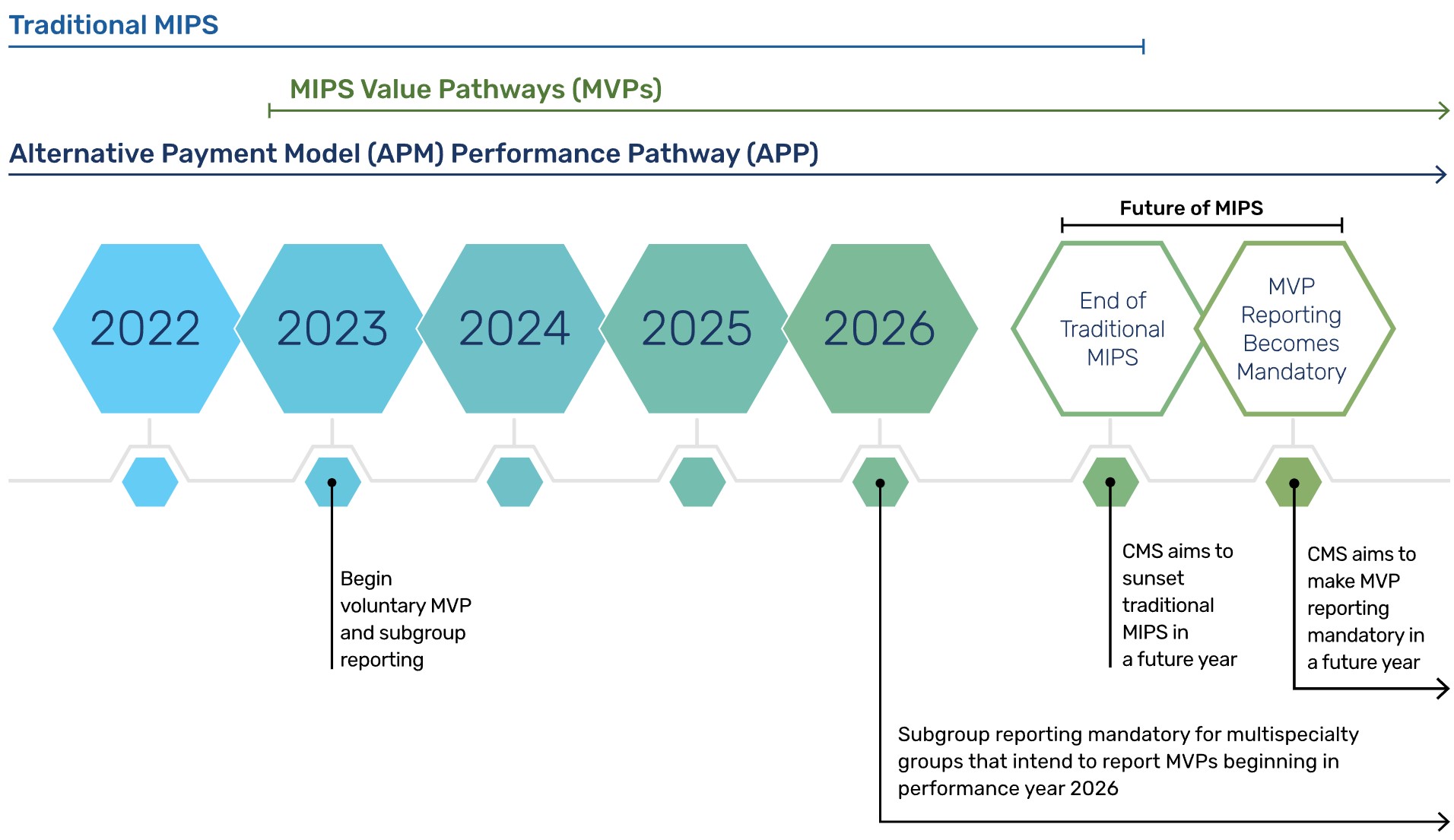
MIPS Value Pathways (MVPs) Expansion
For the 2024 performance year, there are 16 MIPS Value Pathways (MVPs) covering various specialties. Looking ahead to 2025, CMS anticipates that with new and existing MVPs, approximately 80 percent of MIPS-eligible clinicians will have applicable MVPs available for reporting. This initiative is part of a broader strategy to enhance specialist involvement in value-based payment models and foster collaboration between specialty and primary care providers. CMS is also exploring a new model for specialists in ambulatory settings that would utilize the MVP framework. In this proposed model, participants would not receive a traditional MIPS payment adjustment. Instead, their payment adjustment would be based on their performance on a set of clinically relevant MVP measures and their final score compared to a select group of peers in the same specialty and clinical profile who also report on those measures.
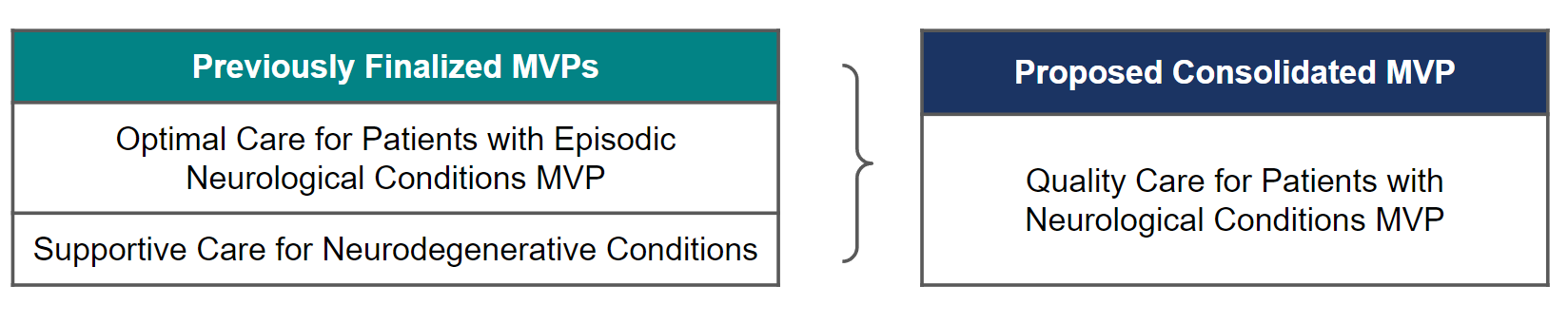
The final rule includes the introduction of six new MVPs and modifications to existing ones. Notably, two neurology-focused MVPs will be consolidated into a single MVP. This consolidation aims to streamline and enhance the focus on neurology-related quality measures. The total number of MVPs will increase to 21 in 2025.
Newly Finalized MVPs for 2025
- Complete Ophthalmologic Care MVP
- Dermatological Care MVP
- Gastroenterology Care MVP
- Optimal Care for Patients with Urologic Conditions MVP
- Pulmonology Care MVP
- Surgical Care MVP
Episode-Based Cost Measures
The Final Rule introduces six new episode-based cost measures and revises two existing ones. These changes are intended to refine the way cost is evaluated within specific clinical episodes, providing a more precise measure of value.
Scoring Adjustments for Topped-Out Measures
CMS finalized a revised methodology for scoring topped-out measures in specialty sets. This adjustment aims to ensure that performance scoring remains relevant and reflective of actual quality improvements. It involves removing the 7-point topped-out measure score cap for clinicians reporting measures included in certain specialty measures and implementing a benchmarking strategy for affected measures that ensures clinicians with limited measure choices and those choosing MVPs are not unfairly penalized.
Flat Benchmarking Methodology
A flat benchmarking methodology will be used for a subset of topped-out measures. Additionally, Medicare Clinical Quality Measures (CQMs) used by Accountable Care Organizations (ACOs) will be scored with flat benchmarks for the 2024 and 2025 performance periods. This means that CMS will not adjust for differences in patient populations, case mix, or other contextual factors for two years.
2025 MIPS Quality Measures Changes
The final rule for the CY 2025 Physician Fee Schedule (PFS) includes several important updates to the MIPS quality measures:
- The final CY 2025 Physician Fee Schedule (PFS) includes nine new MIPS quality measures, including 2 Patient Reported Outcome (PRO) Measures. Here is a list of new measures:
- Excessive Radiation Dose or Inadequate Image Quality for Diagnostic Computed Tomography (CT) in Adults (Clinician Level) – Approved in 2024 Final Rule but deferred (Quality ID 494, eCQM CMSl056v2)
- Positive PD-L1 Biomarker Expression Test Result Prior to First-Line Immune Checkpoint Inhibitor Therapy (Quality ID 506)
- Appropriate Germline Testing for Ovarian Cancer Patients (Quality ID 507)
- Patient-Reported Pain Interference Following Chemotherapy among Adults with Breast Cancer (PRO measure)
- Patient-Reported Fatigue Following Chemotherapy among Adults with Breast Cancer (PRO measure)
- Adult COVID-19 Vaccination Status (Quality ID 508)
- Melanoma: Tracking and Evaluation of Recurrence (Quality ID 509)
- First Year Standardized Waitlist Ratio for Dialysis Patients (FYSWR) (Quality ID 510)
- Percentage of Prevalent Patients Waitlisted (PPPW) and Percentage of Prevalent Patients Waitlisted in Active Status (aPPPW) (Quality ID 511)
- The rule contains substantial changes to 66 existing measures to better align with current best practices and emerging healthcare standards.
- 11 MIPS quality measures are removed for 2025:
- 436 – Radiation Consideration for Adult CT: Utilization of Dose Lowering Techniques (previously finalized for removal with one-year delay)
- 104 – Prostate Cancer: Combination Androgen Deprivation Therapy for High Risk or Very High Risk Prostate Cancer: Percentage of patients
- 137 – Melanoma: Continuity of Care – Recall System
- 144 – Oncology: Medical and Radiation – Plan of Care for Pain
- 254 – Ultrasound Determination of Pregnancy Location for Pregnant Patients with Abdominal Pain
- 260 – Rate of Carotid Endarterectomy (CEA) for Asymptomatic Patients, without Major Complications (Discharged to Home by Post-Operative Day #2)
- 409 – Clinical Outcome Post Endovascular Stroke Treatment
- 433 – Proportion of Patients Sustaining a Bowel Injury at the time of any Pelvic Organ Prolapse Repair
- 439 – Age Appropriate Screening Colonoscopy
- 452 – Patients with Metastatic Colorectal Cancer and RAS (KRAS or NRAS) Gene Mutation Spared Treatment with Anti-epidermal Growth Factor Receptor (EGFR) Monoclonal Antibodies
- 472 – Appropriate Use of DXA Scans in Women Under 65 Years Who Do Not Meet the Risk Factor Profile for Osteoporotic Fracture
ACO Quality Reporting Updates
The 2025 Final Rule introduces important changes for ACO Quality Reporting. Stay tuned for our next blog exploring these changes.
For more information on the CY 2025 Physician Fee Schedule final rule, CMS has published a Fact Sheet.