Submit:
- Two quarters of data for 4 eCQMs to
- QualityNet Secure Portal or with a third party vendor
- Deadline February 28, 2022
2020 taught us that partnerships are vital to successful, stress-free submission. We are happy to be your partner for the 2021 Hospital Inpatient Quality Reporting (IQR) program.
As an eligible facility, you should participate to avoid a 25% reduction of your yearly Annual Payment Update (APU) increase. Failure to participate will also exclude you from the Hospital VBP Program.
There have been some significant changes in the program for 2021 as determined in the FY 2021 IPPS/LTCH PPS final rule, effective October 1, 2020. The new rule mandates progressively increasing the numbers of quarters of eCQM data reported, from one self-selected quarter of data to four quarters of data. The requirements will roll out over a three-year period:
- Two-quarters of data for the CY 2021 reporting period/FY 2023 payment determination
- Three-quarters of data for the CY 2022 reporting period/FY 2024 payment determination
- Four quarters of data beginning with the CY 2023 reporting period/FY 2025 payment determination and for subsequent years, while continuing to allow hospitals to report:
The eCQM-related policies are aligned with proposals under the Promoting Interoperability Program. In another new development, CMS plans to publicly report eCQM performance data on Hospital Compare, beginning with data reported by eligible hospitals and CAHs for the CY 2021 reporting period.
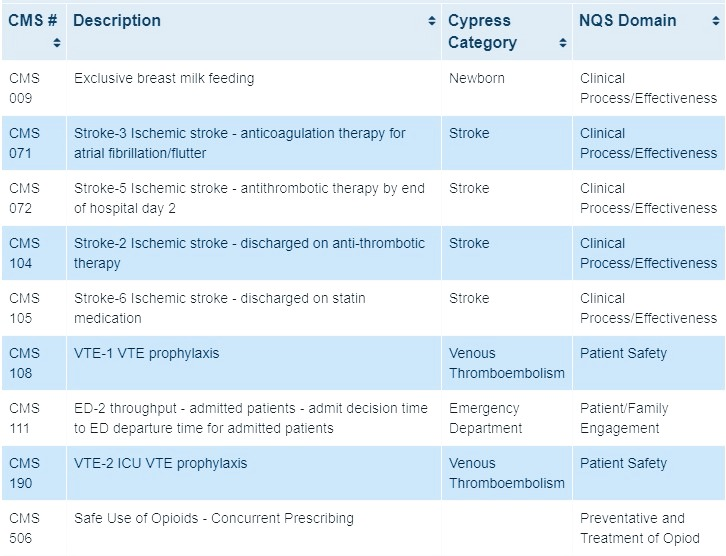
2021 Reporting Period EH/Critical Access Hospitals eCQMs
Hybrid Measures

There is a new voluntary Hybrid Measure for the 2021reporting period: The Hybrid Hospital Wide Readmission (HWR) measure. Hybrid measures merge electronic health record data with claims data to calculate measure results.
Hospitals that submit data for this measure during the reporting period will receive confidential facility-specific reports that detail submission results, as well as the Hybrid HWR measure results. Data will not be publicly reported during the voluntary reporting period. CMS will publicly report the Hybrid HWR measure results beginning with data collected from July 1, 2023, through June 30, 2024 reporting period. Note that this voluntary hybrid measure does not count toward eCQM submission:

Third-Party Vendor Requirements
The requirements for your Third-party Vendor/EHR for reporting 2021 data is that they must be 2015 Edition certified with the most current measure version of the eCQM specifications. They have also expanded the requirement to use EHR technology certified to the 2015 Edition for submitting data on not only the previously finalized Hybrid Hospital-Wide Readmission measure but all hybrid measures in the Hospital IQR Program.
Last year, DHIT successfully certified CQMsolution for the 2015 Edition Cures Update with all eCQMs and we have been approved as 2021 Qualified Registry. We have taken the lead with certification and our partners are prepared for 2021. If you would like to partner with us for quality measures or as your third-party vendor, please contact us today. Stay tuned for our 2021 Joint Commission ORYX blog outlining all the changes!