In our past blog, Surprise Changes to QPP for 2021, we briefly explained Alternative Payment Models (APMs) and APM Performance Pathways (APPs). In our role as Strategic Partner to many Electronic Health Record (EHR) vendors, we have fielded many questions regarding APP support, so we will delve deeper in this blog.
Understanding Alternative Payment Models (APMs)
APMs are alternatives to the traditional Merit-Based Incentive Payment System (MIPS) and fee-for-service reimbursement that may offer benefits to clinicians beyond those offered by MIPS.

Any of these programs offer physician practices the opportunity for enhanced reimbursement in exchange for taking an additional measure of risk above and beyond MIPS. The APP was designed with the goal of reducing the reporting burden, encouraging participation in APMs and creating new scoring opportunities for MIPS APMs.
APM Performance Pathway Requirements
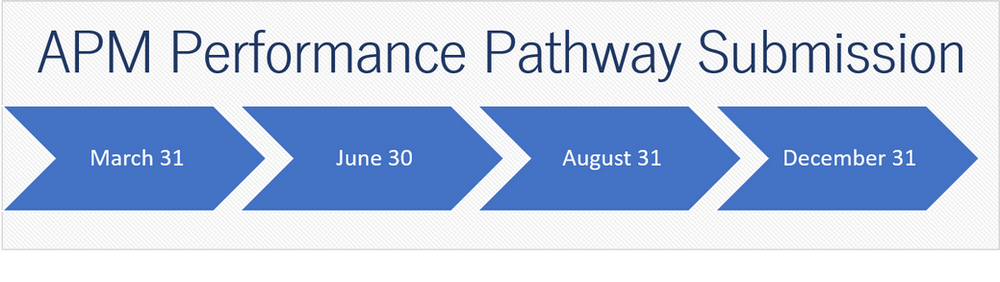
APM participants must be MIPS eligible and they can submit as an eligible clinician, group (TIN), or MIPS APM Entity. Beginning in the 2023 performance year, MIPS eligible clinicians will be allowed to report to the APP as a subgroup, “a subset of a group which contains at least one MIPS eligible clinician and is identified by a combination of the group TIN, the subgroup identifier, and each eligible clinician’s NPI.” Only MIPS APM participants have the option to report via the new APP on any of the four snapshot dates ( March 31, June 30, August 31, and December 31) during the performance period. APP is required for all Medicare Shared Savings Program Accountable Care Organizations (MSSP ACOs).
For 2022, MIPS APMs are required to submit a full year of data for the Quality performance category, Promote Interoperability by electronic exchange of information by use of CEHRT and patient engagement, and 90-days of data for Improvement Activities—unless otherwise specified within the activity.
APP Performance Categories and Scoring
Three performance categories make up your final score when reporting through the APP:
- Quality 50% of MIPS final score
- Promoting Interoperability (PI) 30% of the MIPS final score
- Improvement Activities (IA) 20% of the MIPS final score, although all APP participants will automatically get the full 20% regardless of actual Improvement Activities
All participants submitting to the APP report on the same set of six quality measures, shown below:
| Measure Number | Measure Title | Collection Type | Submitter Type |
| Quality ID#: 001 | Diabetes: Hemoglobin A1c (HbA1c) Poor Control | eCQM/MIPS CQM/CMS Web Interface | APM/Entity/Third Party Intermediary |
| Quality ID#: 134 | Preventive Care and Screening: Screening for Depression and Follow-up Plan | eCQM/MIPS CQM/CMS Web Interface* | APM/Entity/Third Party Intermediary |
| Quality ID#: 236 | Controlling High Blood Pressure | eCQM/MIPS CQM/CMS Web Interface* | APM/Entity/Third Party Intermediary |
| Quality ID#: 321 | CAHPS for MIPS | CAHPS for MIPS Survey | Third Part Intermediary |
| Quality ID#: 479 | Hospital-Wide, 30-day, All-Cause Unplanned Readmission (HWR) Rate for MIPS Eligible Clinician Groups | Administrative Claims | N/A |
| Quality ID#: TBD | Risk Standardized, All Cause Unplanned Admissions for Multiple Chronic Conditions for ACOs | Administrative Claims | N/A |
Medicare Shared Savings Program ACOs
In response to concerns from ACOs, CMS has extended the CMS Web Interface as a reporting option for ACOs for 3 years through the performance year 2024. ACO’s will be required to report the 3 eCQMs (above) beginning in the performance year 2025. Another delay for ACOs is the quality performance standard as they are maintaining the MIPS quality performance score of 30% for the 2023 performance year. In order for ACOs to meet the Shared Savings Program they must:
- Report Quality via APP
- Report 10 measures under the CMS Web Interface or 3 eCQMs/MIPS CQMs.
- 6 of 10 measures must have data completeness
- all 3 must have data completeness
- 2022 and 2023 Incentives for reporting eCQMs/MIPS CQMs
- Must achieve 30% or higher across all MIPS quality categories
MIPS APP Submission Requirements
With so many CMS programs available, EHRs should have an understanding of their users’ support needs. Primary Care First (PCF) is another type of MIPS APM that has its own set of required CQMs and a specific QRDA III output format. Before your users can participate as an APM and the APP they should consider whether your software can support the QRDA III reporting/output requirements. Some users will utilize a Qualified Registry or QCDR, but they still need to confirm the Third-party Intermediary offers this support. If the participant is self submitting, the EHR or eCQM reporting software must provide a QRDA III or QPP JSON with the following:
- Alternative Payment Model (APM) Entity Identifier
- Required for MIPS APM Entity reporting
- Required for APP APM Entity reporting
- For PCF, this is the PCF Practice Site Identifier assigned by PCF
| CMS Program Name | Code |
| Primay Care First | PCF* |
| MIPS Individual | MIPS_INDIV |
| MIPS Group | MIPS_GROUP |
| MIPS Virtual Group | MIPS_VIRTUALGROUP |
| MIPS APM Entity | MIPS_APMENTITY* |
| MIPS APP Individual Reporting | MIPS_APP1_INDIV |
| MIPS APP Group Reporting | MIPS_APP1_GROUP |
| MIPS APP APM Entity | MIPS_APP1_APMENTITY |
These data elements must be present in the QRDA III XML or JSON output from your EHR, per the CMS Implementation Guide.
EHR APM Performance Pathway Support Checklist
- Review your currently supported quality measures
- Add APM Identifier
- Increase your QRDA III reporting/output to support submission to:
- APP Portal User Interface
- API
- Part B Claims (when applicable)
- Web Interface for MSSP ACOs
- Provide participants an optional partner for reporting with a Qualified Registry
DHIT CQMsolution and Dynamic Registry
DHIT has added the program specific output to CQMsolution and coupled with our Dynamic Registry platform, your users will have a complete APP solution. For more information, please contact us or visit, APM Performance Pathway – QPP (cms.gov).