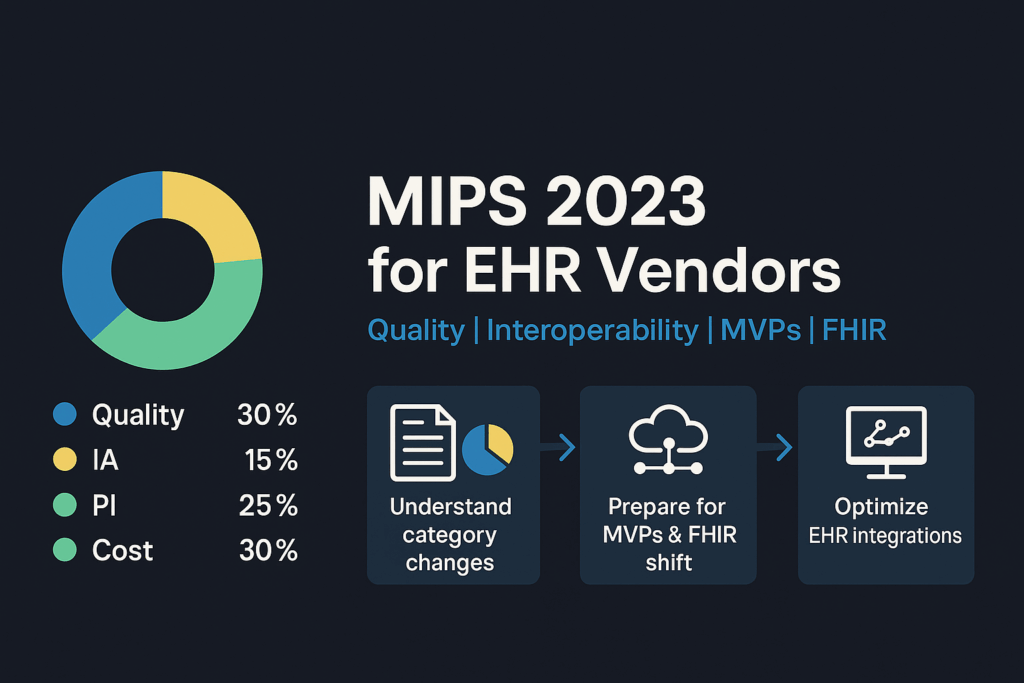
For 2023 CMS fine-tunes the MIPS program and, in particular, makes some changes to the quality reporting component while slowly transitioning towards its two major quality reporting objectives:
- MIPS Value Pathways (MVPs), and
- The migration of Clinical Quality Measures to FHIR
MVPs Introduction
MVPs are CMS’ initiative to tailor the MIPS program to be more relevant to a clinicians area of practice. They are optional for 2023. Each MVP has a limited set of measures that focus on a particular medical specialty (e.g. Cardiology has an “Advancing Care for Heart Disease MVP) or medical condition (e.g. cancer). Since we are quality measure experts, we will focus on Quality reporting requirements for 2023 and gotchas for 2022 Quality reporting.

Category Weighting and Performance Thresholds
Overall MIPS thresholds remain the same as for 2022. To avoid a penalty, you must score at least 75 points. Non-participation or a low score can result in a 9% penalty on Medicare reimbursement. Since the MIPS program is budget-neutral, the maximum bonus is 9%, to be applied to your 2025 Medicare reimbursement.
Quality Measure Reporting
For 2023, there are nine new measures, including one administrative claims measure, one composite measure, five high-priority measures, and two patient-reported outcomes measures. A couple of notable new measures include Psoriasis and Dermatitis.
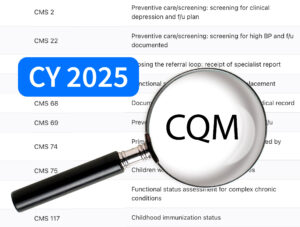
In the 2022 reporting year, 200 CQMs were available. For 2023, there will be 198 CQMs to choose from, as some old measures were removed and some new ones added:
New Quality Measures for 2023:

Retired Measures:

CQM 110 Status Clarification:

It has been removed as a measure for traditional MIPS (Quality # 110) but retained as a measure for ACOs and as an eCQM for MVPs.
Truncated and Suppressed Quality Measures – Flashback to 2022
CMS recognized that some quality measures were impacted by the October 2022 ICD-10 code update. Since quality measure specifications can’t be updated during the current performance period, these measures will be suppressed (eCQMs) or truncated (MIPS CQMs and claims-based measures). What does that mean to you?
Suppressed CQMs:
- CMS will exclude the points from this measure – the denominator is reduced by 10 points and the numerator is excluded from scoring.
- If a suppressed measure is one of the 6 CQMs you submit, your Quality category denominator will be reduced by 10 points. Out of the remaining measures you submit, CMS will use your highest scoring outcome/high priority measure and 4 remaining highest scoring measures.

Truncated CQMS:
- For these measures CMS will only use data from the first 9 months of the year (prior to October 1, 2022). Only data from January through the end of September will be counted.

Quality Scoring Changes
Prior to 2023, CQMs had a 3-point floor, so if you reported on a CQM, 3 points was the minimum score per measure. Except for small practices (<16 clinicians) this is no longer the case. Measures:
- With a benchmark,
- Meeting the 20-case minimum, and
- Data completeness
Will be scored on a 1-10 scale. Measures failing any of these criteria will earn 0 points for larger practices and 3 points for small practices.
DHIT Solutions for MIPS Compliance
As outlined in our earlier discussion of MVPs, CMS is transitioning toward a specialty-focused approach for the Quality Payment Program. At Dynamic Health IT (DHIT), we are committed to positioning our Strategic Partners ahead of this transformation through our comprehensive Qualified Registry and our ONC-certified Cures Update 2023 version of CQMsolution.
We support quality measures for various medical specialties, including radiology, oncology, behavioral health, primary care and others. Our annual CQMsolution updates keep you up-to-date with measure changes. Stay tuned for future blogs on MVPs and FHIR-based CQMs.