The Centers for Medicare and Medicaid Services (CMS) issued their Final Rule for the 2022 Medicare Physician Fee Schedule (PFS) on November 2, 2021 and it includes changes to the Quality Payment Program (QPP). CMS made some significant revisions to the current MIPS program and continues to lay the foundation for MIPS Value Pathways (MVPs) and the migration of Clinical Quality Measures to FHIRⓇ. Since we are quality measure experts, we will focus on Quality reporting requirements for 2022.
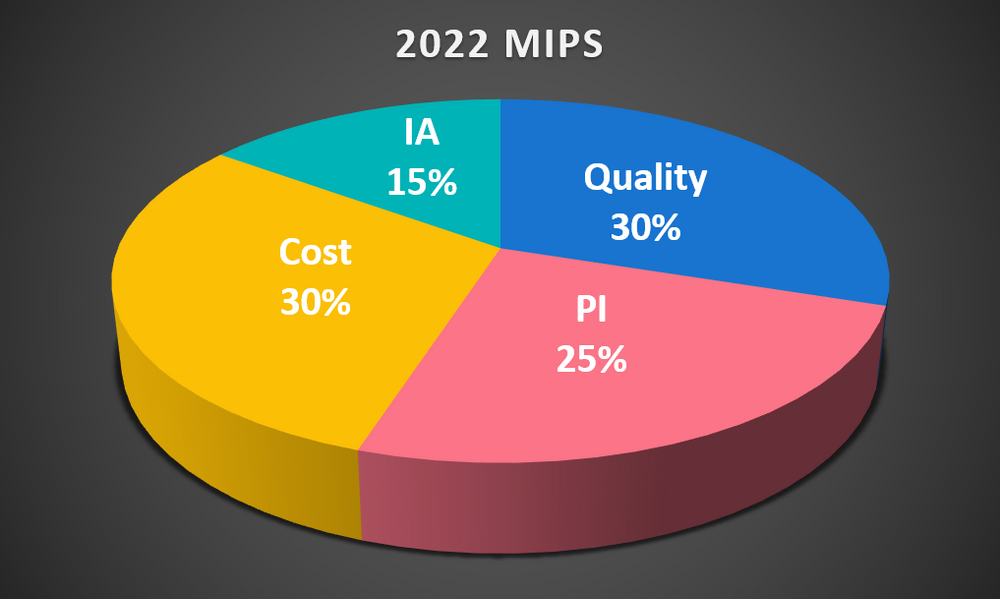
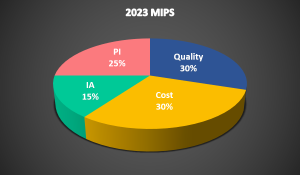
Category Weighting and Performance Thresholds
As mandated in the MACRA legislation, the Quality and Cost performance categories are weighted equally at 30% starting in 2022. Also, the performance threshold has increased. To avoid a penalty, you must score at least 75 points. Non-participation or a low score can result in a 9% penalty on Medicare reimbursement. To qualify for Exceptional Performance and receive up to a 9% bonus, you must score at least 89 points.
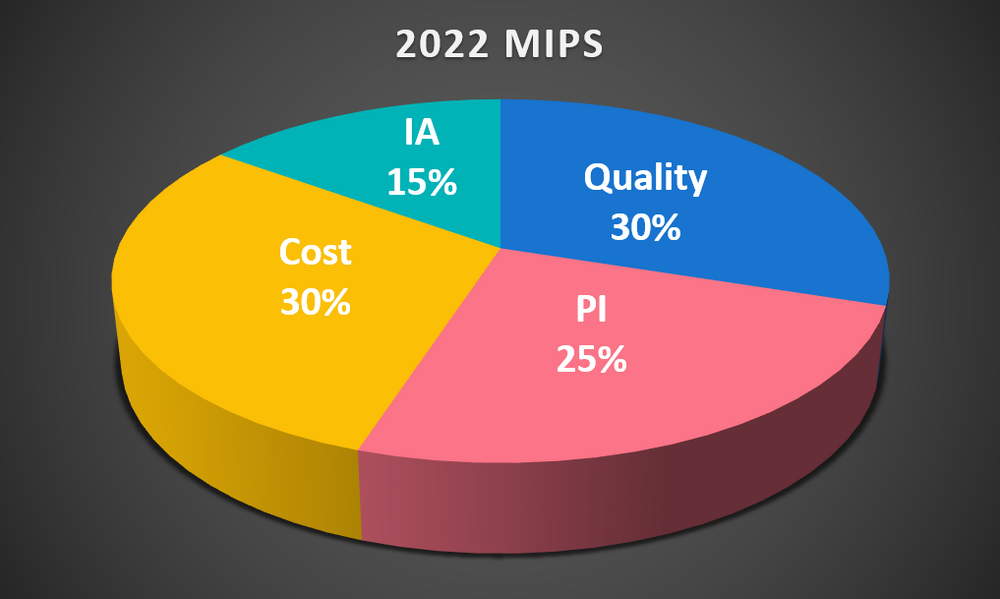
Note that the weightings for Promoting Interoperability (PI) and Improvement Activities (IA) have not changed from 2021.
Quality Measure Reporting
For 2022, bonus points are no longer available for end-to-end reporting, high-priority measures or outcomes-based measures. CMS did decide to extend availability of the CMS Web Interface for MIPS Alternative Payment Model (APM) participants. Also, there were some Clinical Quality Measure (CQM) changes.
In the 2021 reporting year, 209 CQMs were available. For 2020, there will be 200 CQMs to choose from, as some old measures were removed and some new ones added:
New Measures
| MIPS # | CMS # | Measure Description |
| 481 | 646 | Intravesical Bacillus-Calmette Guerin for Non-muscle Invasive Bladder Cancer |
| 482 | N/A | Hemodialysis Vascular Access: Practitioner Level Long-term Catheter Rate |
| 483 | N/A | Person-Centered Primary Care Measure Patient-Reported Outcome Performance Measure (PCPCM PRO-PM |
No eCQMs were removed but CMS did remove some claims-based measures:
Removed Measures
| MIPS # | Measure Description |
| 14 | Age-Related Macular Degeneration (AMD): Dilated Macular Examination for Medicare Part B Claims type only |
| 21 | Perioperative Care: Selection of Prophylactic Antibiotic – First OR Second-Generation Cephalosporin |
| 23 | Perioperative Care: Venous Thromboembolism (VTE) Prophylaxis (When Indicated in ALL Patients) |
| 44 | Coronary Artery Bypass Graft (CABG): Preoperative Beta-Blocker in Patients with Isolated CABG Surgery |
| 50 | Urinary Incontinence: Plan of Care for Urinary Incontinence in Women Aged 65 Years and Older for Medicare Part B Claims type only |
| 67 | Hematology: Myelodysplastic Syndrome (MDS) and Acute Leukemias: Baseline Cytogenetic Testing Performed on Bone Marrow |
| 70 | Hematology: Chronic Lymphocytic Leukemia (CLL): Baseline Flow Cytometry |
| 154 | Falls: Risk Assessment |
| 195 | Radiology: Stenosis Measurement in Carotid Imaging Reports |
| 225 | Radiology: Reminder System for Screening Mammograms |
| 337 | Psoriasis: Tuberculosis (TB) Prevention for Patients with Psoriasis, Psoriatic Arthritis and Rheumatoid Arthritis on a Biological Immune Response Modifier |
| 342 | Pain Brought Under Control Within 48 Hours |
| 429 | Pelvic Organ Prolapse: Preoperative Screening for Uterine Malignancy |
| 434 | Proportion of Patients Sustaining a Ureter Injury at the Time of Pelvic Organ Prolapse Repair |
| 444 | Medication Management for People with Asthma |
You may have noticed CMS shifting towards a specialty-focused orientation for the Quality Payment Program. At Dynamic Health IT (DHIT), we are working to keep our Strategic Partners ahead of this shift with our Qualified Registry and the ONC-certified Cures Update version of CQMsolution for the 2022 reporting period. We support quality measures for various medical specialties, including radiology, oncology, behavioral health, primary care and others.
Looking Towards the Future
MIPS Value Pathways (MVP’s)
In spite of all the disruption from COVID, CMS is still moving towards implementation of MVPs. They will gradually replace the “traditional” MIPS program, as clinicians will be able to report MVPs beginning with the 2023 performance year. MVPs will start as voluntary participation for the 2023 through 2027 performance years.
MVPs contain specific measures from the Quality, Improvement Activities and Cost categories, which together make up the first layer of the MVP framework. The second layer will contain Promoting Interoperability and Population Health measures and will address hospitalizations and readmissions.
Here are the voluntary MVPs proposed for the 2023 reporting period:
- Advancing Rheumatology Patient Care
- Coordinating Stroke Care to Promote Prevention and Cultivate Positive Outcomes
- Advancing Care for Heart Disease
- Optimizing Chronic Disease Management
- Adopting Best Practices and Promoting Patient Safety within Emergency Medicine
- Improving Care for Lower Extremity Joint Repair
- Support of Positive Experiences with Anesthesia
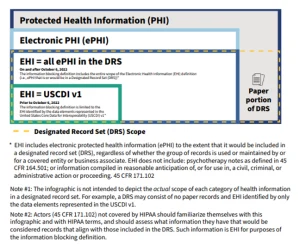
Advancing Quality Measures with FHIR
Moving forward, CMS is planning to transition to FHIR-based eCQMs and “Digital Quality Measures”, which will expand the scope of eCQMs to include electronic (non-abstracted, non-claims-based) data from a variety of sources to augment the data currently pulled from your EHR. Stay tuned for a forthcoming blog about our work with the National Committee for Quality Assurance (NCQA) and FHIR-based measures!